The healthcare industry is undergoing seismic shifts that are causing serious consequences for both patients and providers. As we move through 2024, these changes are becoming increasingly apparent, raising concerns about accessibility, affordability and overall quality of care. We look at 20 worrying trends in the healthcare industry that could affect you:
Rising Healthcare Costs

Healthcare costs in the U.S. have been steadily increasing for years,and 2024 is no exception. The costs of medical procedures, prescription drugs and insurance premiums continue to rise, outpacing inflation and wage growth. This leaves many individuals struggling to afford necessary care.
Increasing Insurance Premiums

Many people are facing higher insurance premiums, with some plans becoming unaffordable. This has forced some individuals to opt for less comprehensive plans, leaving them vulnerable to high out-of-pocket costs in case of a medical emergency.
Lack of Transparency in Pricing

Despite calls for more transparency, many healthcare providers and insurers still do not provide clear, upfront pricing for services. Patients often face unexpected bills for procedures, lab tests, or doctor visits due to hidden fees or complex billing systems.
The Staffing Crisis

There is a growing shortage of healthcare professionals, including nurses, physicians and technicians. The pandemic exacerbated burnout and many professionals have left the field. As a result, patients may experience longer wait times, rushed consultations, and reduced access to care.
Telehealth Limitations

While telehealth boomed during the pandemic, regulatory and reimbursement challenges are now limiting its growth. Some insurance companies have reduced coverage for virtual appointments, and states are rolling back emergency provisions that allowed telehealth across state lines.
Consolidation of Healthcare Systems

More healthcare facilities are merging, leading to fewer independent hospitals and clinics. While consolidation can improve resource allocation, it often reduces competition, which can drive up costs for patients and limit choices for care.
Rising Prescription Drug Prices
The cost of prescription drugs continues to soar, with many new drugs entering the market at exorbitant prices. While some progress has been made in negotiating prices, many patients still struggle to afford essential medications, especially for chronic conditions.
Increased Reliance on Technology

Artificial intelligence (AI) and machine learning are increasingly being integrated into healthcare. While this can improve diagnostics and treatment plans, it raises concerns about data privacy, job displacement for healthcare workers and the depersonalization of patient care.
Data Breaches and Cybersecurity Risks

Healthcare providers are prime targets for cyberattacks due to the sensitive nature of patient data. In 2024, the frequency and severity of data breaches are increasing, putting personal health information at risk. This has led to identity theft and other forms of fraud for affected patients.
Medical Debt

Medical debt remains a major issue in the U.S., with millions of Americans owing thousands of dollars in unpaid medical bills. Even insured individuals are often caught off guard by high deductibles, co-pays and out-of-network charges, leading to financial stress and potential bankruptcy.
Healthcare Disparities

Disparities in healthcare access and quality persist, particularly for racial minorities, low-income individuals and rural communities. These groups often face barriers to care, including fewer healthcare facilities, higher rates of uninsured individuals and worse health outcomes.
Delays in Non-Emergency Care

Due to staffing shortages and increasing demand, non-emergency procedures, such as elective surgeries and specialist appointments, are often delayed. This can lead to deteriorating health conditions and prolonged pain or discomfort for patients waiting for care.
Mental Health Crisis

The mental health crisis is escalating, with more people seeking care for anxiety, depression, and other mental health disorders. But, the demand for mental health professionals far exceeds the supply, leaving many patients unable to access timely and effective treatment.
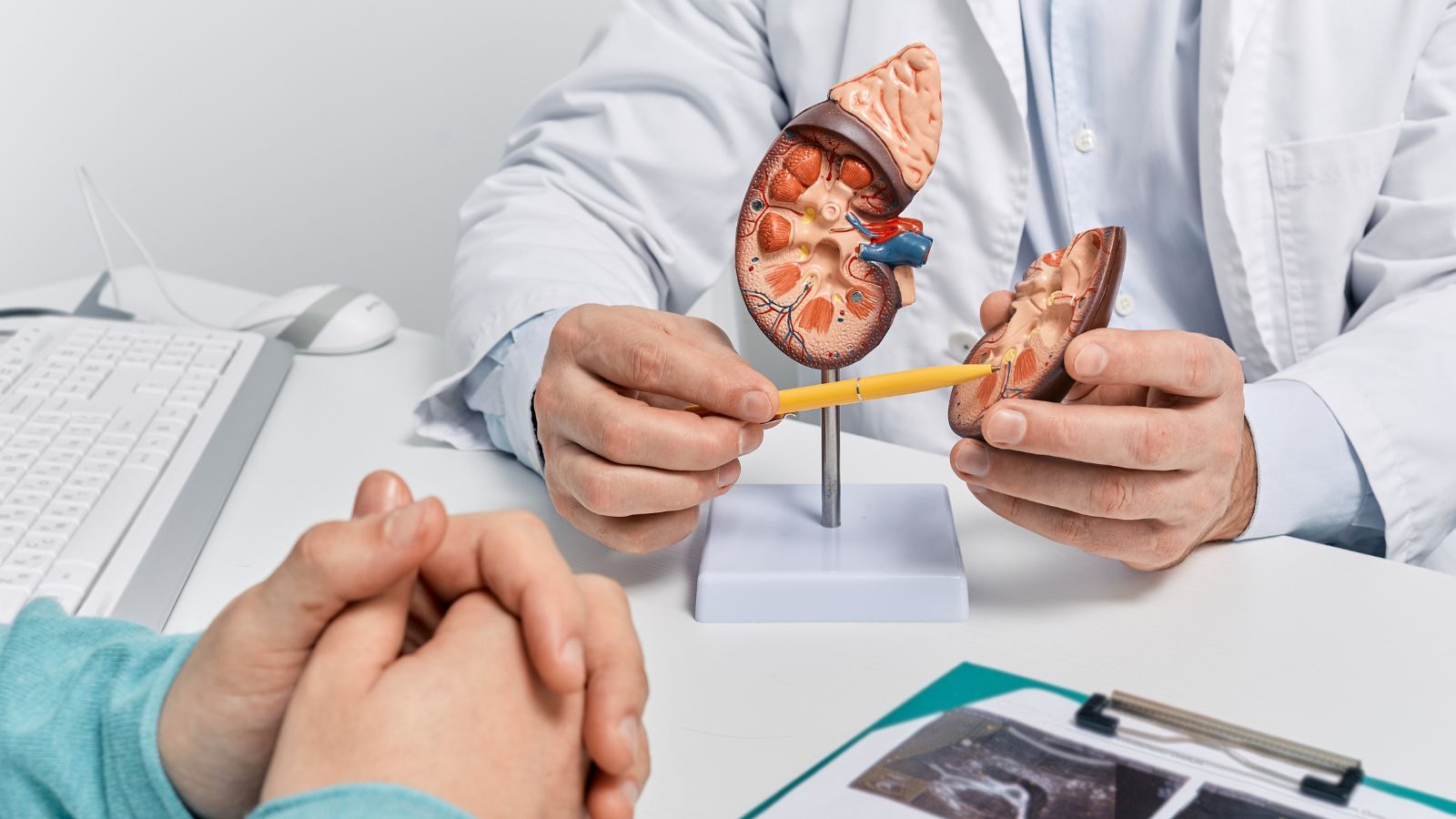
Lack of Access to Specialized Care

In many regions, particularly rural areas, access to specialists like oncologists, cardiologists, and neurologists is limited. Patients often have to travel long distances or wait extended periods to see a specialist, delaying critical diagnoses and treatment.
The Impact of Climate Change

Climate change is affecting public health, with more frequent and severe heatwaves, wildfires and natural disasters leading to an increase in health emergencies. Healthcare facilities are also being challenged by climate-related infrastructure issues, such as flooding and power outages.
Growing Role of Private Equity

Private equity firms are increasingly investing in healthcare providers, including nursing homes, hospitals and physician practices. While this can bring in necessary capital, there are concerns that profit-driven motives may compromise patient care and lead to cost-cutting measures that reduce quality.
Shifting Policies on Reproductive Health
Legislation and court rulings around reproductive health are creating a fragmented landscape of care across the U.S. Access to abortion and other reproductive services has been restricted in many states, leaving individuals in certain regions with limited options for necessary healthcare.
Changes in Medicare and Medicaid

Government programs like Medicare and Medicaid are facing financial pressure. Changes in reimbursement rates, eligibility and covered services could limit access for vulnerable populations, including the elderly, disabled and low-income individuals.
The Rise of Direct-to-Consumer Healthcare

More companies are offering direct-to-consumer healthcare services, such as telemedicine platforms and home testing kits. While this can increase convenience, there are concerns about the quality of care and oversight, especially with unregulated or unvetted providers.
Healthcare Worker Burnout

Burnout among healthcare workers has reached unprecedented levels, leading to mass resignations and early retirements. This exodus of experienced professionals is creating a skills gap, reducing the quality of care and increasing the workload on remaining staff, further exacerbating the burnout cycle.
18 Reasons Why People Are Leaving Florida in Masses

Exploring factors that impact the desirability of living in Florida, this list delves into various challenges shaping residents’ experiences. From environmental concerns like rising sea levels to economic factors such as fluctuating job markets, these issues collectively contribute to a nuanced understanding of the state’s appeal.
18 Reasons Why People Are Leaving Florida in Masses
